What is pulp necrosis, and how should it be treated?
Slowly, a tooth turns black. Maybe it is a slow process, but this can be the symptom of a particular condition, namely dental necrosis. This means that the tooth dies from a cause that can and should be investigated. But it is also a wake-up call to immediately reach your trusted dentist and book a visit: you need to avoid toothaches linked to the effects of pulpal necrosis.
What is dental necrosis?
It is a pathology that involves the terminal phase of the parts known as dental pulp. A tooth goes into necrosis when the soft tissues, its vital part, are dead. This condition occurs because the nerves and blood vessels that compose it are irreversibly damaged for different causes.
Despite being a condition from which there is no turning back, dental necrosis must still be treated correctly. This is to avoid annoying and painful consequences.
Symptoms and causes of dental necrosis
The causes of dental necrosis are different. In many cases, the death of a tooth was caused by a strong trauma that affected the tooth at the pulp level or by a cavity that was not treated in time.
Understanding if a tooth is in the necrotic phase is not always easy and immediate. In any case, there are some symptoms to pay attention to that can be a warning sign for the patient.
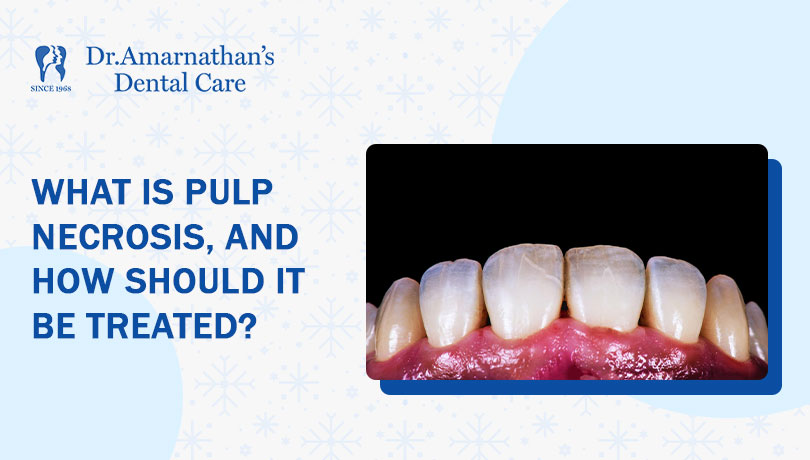
1)Tooth color
The first sign that can warn us that the tooth is dying is the change in color. In fact, in case of necrosis, the tooth will tend to become darker or take on a yellow or gray color.
This is due to the blood pigmenting the tooth a bit, like when a bruise forms on the knee following a trauma. A necrotic tooth turns black only if it is not treated. Or it is treated inadequately, and as a result, the color change increases over time.
2)The Pain
A second symptom of dental necrosis is the progressive growth of painful sensation. The level of perceived pain increases as the state of necrosis progresses. While it may be almost non-existent at the beginning, over time, the pain becomes more intense and persistent.
If the patient experiences the presence of these symptoms, he must book a visit to his dentist who, based on the diagnosis, decides whether to carry out a root canal treatment or extract it.
How to cure dental necrosis
Treatment of dental necrosis can vary based on its level of advancement. Generally, after carefully examining the patient, the dentist can decide whether to devitalize the tooth or extract it.
This second hypothesis is taken into consideration much more rarely. It is generally preferred to proceed with root canal treatment, a conservative measure that, if carried out with a rubber dam and the use of an electron microscope, offers completely predictable and controlled results.
Even in cases where a cavity has affected the roots under the gum, the tooth can often be treated and saved. This is done by lowering the gum around it with periodontal surgery.
Devitalization
Dental root canal treatment is a root canal treatment with the removal of dental pulp and necrotic tissue from the tooth canals. First of all, the pulp is extracted, and both the cavity and the root canals are carefully cleaned. Subsequently, these are filled with bio-compatible material (for example, gutta-percha), and finally, the tooth is reconstructed with composite material.
The treatment is not painful; it is done under anesthesia, and in most cases, the operative course does not cause problems. The failure of a root canal over time depends most of the time on the failure to use the rubber dam. Or a magnifying system while running.
Extraction
Extracting the tooth always represents a second choice, which is practiced only when the tooth cannot be saved. Typically, after the extraction, dental implant surgery is performed to restore functionality and aesthetics to the patient’s smile.
Neglected necrosis, what are the consequences?
The state of dental necrosis should not be overlooked as it can cause annoying consequences such as infections in the bone. Among the most common complications of untreated necrosis are:
- Apical abscess, pus at the root of a tooth caused by an infection that has spread from the tooth to the tissues.
- Apical granuloma is a chronic inflammation of the tissues surrounding the root apex.
- Radicular cysts are root cysts that develop following infectious pathologies of the internal tissues.
- Apical periodontitis is inflammation of the periodontium following inflammation of the pulp.
So, what should one do if a tooth is in necrosis, then? To avoid the tooth becoming black and getting painful, seeing the dentist regularly is undoubtedly the first practical approach. Then, we must take action as quickly as we can.
Winding it up
In conclusion, pulp necrosis is a dangerous dental disorder that has to be treated right away. Recognizing the early signs, such as changes in tooth color and increasing pain, is crucial for early intervention. Neglecting dental necrosis can lead to severe complications and infections in the bone, making early treatment imperative.
Treatment options, including root canal therapy and, as a last resort, tooth extraction, should be discussed with a trusted dentist based on the extent of the condition. Root canal treatment, when performed with precision and care, can effectively address dental necrosis and save the affected tooth, providing predictable and controlled results.
Regular dental check-ups and prompt action are key to preventing the progression of dental necrosis and its associated discomfort and health risks. Taking proactive steps to address this condition ensures the preservation of dental health and overall well-being.