Is Burning Mouth Syndrome a Dental Concern? Understanding Its Impact on Oral Health
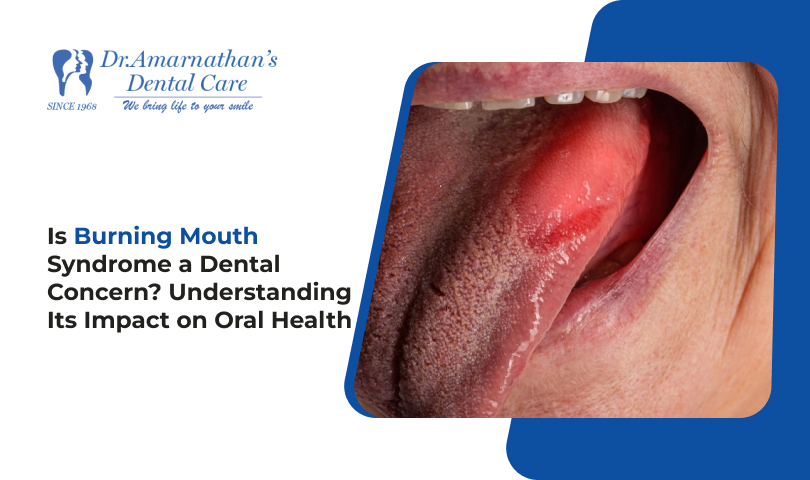
Burning Mouth Syndrome (BMS) can significantly impact an individual’s quality of life. It is characterized by a burning sensation in the mouth, often affecting the tongue, lips, and roof of the mouth. This feeling may vary from mild discomfort to severe pain, and it can occur without any visible signs or abnormalities in the oral cavity.
In this comprehensive blog post, we will explore Burning Mouth Syndrome, its potential causes, symptoms, and, most importantly, how it relates to oral health. If you or someone you know is experiencing unexplained burning in the mouth, this guide will provide valuable insights into how this condition can be managed and treated.
What is Burning Mouth Syndrome (BMS)?
Burning Mouth Syndrome is a chronic condition that causes a persistent burning sensation in the mouth, often without any obvious cause. Unlike some oral conditions, BMS is not always linked to a visible change in the mouth. It typically affects the tongue, but it can also involve other parts of the mouth, including the roof of the mouth, lips, gums, or inside the cheeks.
The sensation is often described as feeling like a hot or scalded mouth, and it may come and go, sometimes lasting for months or even years. BMS can affect people of all ages but is most common in middle-aged or older adults, particularly women, and it tends to worsen as people age.
How is Burning Mouth Syndrome Diagnosed?
Diagnosing Burning Mouth Syndrome can be challenging, as there are no specific tests to confirm the condition. Instead, dentists and medical professionals typically diagnose BMS by eliminating other possible causes, such as:
- Oral infections (like thrush or cold sores)
- Dental problems (e.g., tooth decay, gum disease)
- Nutritional deficiencies
- Medications (side effects)
- Hormonal changes (especially during menopause)
Your dentist will also conduct a thorough examination of your oral cavity, take a detailed health history, and may refer you to other healthcare professionals, such as an endocrinologist or neurologist, for further evaluation.
What Causes Burning Mouth Syndrome?
The exact cause of Burning Mouth Syndrome remains unclear, but several factors may contribute to the condition. These include:
- Oral Health Issues
- Dry Mouth (Xerostomia): Saliva plays a key role in protecting the tissues in your mouth. A lack of saliva due to certain medications, dehydration, or other factors can lead to a dry mouth, which may trigger or worsen BMS.
- Tooth Sensitivity: People with tooth sensitivity or gum recession may experience a burning sensation when exposed to hot, cold, or acidic foods.
- Oral Infections: Fungal infections like candidiasis (thrush) can cause a burning sensation, though these symptoms are often treatable with antifungal medications.
- Hormonal Imbalance
For many individuals, particularly women going through menopause, hormonal changes can play a significant role in the development of BMS. Lower levels of estrogen may affect the taste buds and oral tissues, contributing to the burning sensation.
- Nutritional Deficiencies
Deficiencies in certain vitamins and minerals, such as Vitamin B12, iron, and zinc, can lead to nerve dysfunction and oral discomfort, potentially causing BMS symptoms.
- Psychological Factors
Stress, anxiety, and depression have been linked to an increase in BMS cases. These psychological factors can lead to changes in how the body perceives pain, making the burning sensation more intense.
Is Burning Mouth Syndrome a Dental Concern?
While Burning Mouth Syndrome is often viewed as a medical condition, it has important implications for oral health, and dentists are usually the first to identify it. Here’s how BMS impacts oral health and why dentists should be involved in its diagnosis and management:
1. Impact on Oral Tissues
One of the primary concerns with Burning Mouth Syndrome is its potential to cause oral discomfort, which can interfere with regular activities like eating, speaking, and swallowing. The condition may also be linked to poor oral hygiene due to difficulty in maintaining comfort during brushing or flossing.
2. Dry Mouth (Xerostomia)
Dry mouth is a common symptom of BMS, which can exacerbate oral health issues. Without sufficient saliva, the mouth becomes more prone to tooth decay, gum disease, and bad breath. Therefore, managing dry mouth is critical in the treatment of BMS.
3. Risk of Tooth Sensitivity
BMS can sometimes be confused with or occur alongside tooth sensitivity, making it important for a dentist to evaluate the patient’s overall oral health. Sensitive teeth can further aggravate the symptoms of BMS, especially when eating hot or cold foods.
How is Burning Mouth Syndrome Treated?
There is no one-size-fits-all treatment for Burning Mouth Syndrome. The goal of treatment is to manage symptoms and address any underlying causes that may be contributing to the condition. Below are some common approaches to managing BMS:
- Oral Care and Hygiene
- Good Oral Hygiene: Regular brushing with a soft-bristled toothbrush and fluoride toothpaste can help keep the mouth clean and reduce the irritation caused by BMS.
- Saliva Substitutes: If dry mouth is a concern, your dentist may recommend saliva substitutes or moisturizing mouth sprays.
- Dietary Adjustments
- Vitamin Supplements: If BMS is linked to a nutritional deficiency, vitamin supplements (like B12, iron, or zinc) may be recommended by your dentist or doctor.
- Avoiding Triggers: Certain foods, such as spicy or acidic foods, can aggravate BMS symptoms. Your dentist might suggest avoiding these foods until symptoms improve.
- Medications
In more severe cases, medications like anti-depressants or neuropathic agents (used to treat nerve pain) may be prescribed to help manage symptoms.
- Psychological Support
Stress management techniques and counselling may help alleviate the psychological factors contributing to BMS.
When Should You Visit a Dentist About Burning Mouth Syndrome?
If you experience a persistent or unexplained burning sensation in your mouth, it’s important to consult with your dentist. A dentist can help determine whether the condition is related to oral health problems like dry mouth or infections or requires further medical investigation. Finding and treating the problem early can help control symptoms and prevent future issues.
Conclusion
Burning Mouth Syndrome (BMS) can be a difficult condition to deal with. Although it may not show obvious signs, its effect on oral health should be addressed. Dentists play a crucial role in diagnosing and managing BMS, offering treatments that can help alleviate symptoms and improve quality of life.
By understanding the potential causes and symptoms of BMS and by seeking timely dental care, individuals affected by this condition can better manage their oral health and overall well-being.